A healthy young adult male produces on average about 7-10mg of testosterone every day. The pituitary gland produces a hormone called LH, in response to hypothalamus stimulation, which stimulates the testes to produce testosterone. Normal male aging is accompanied by a decline in testicular function resulting with a fall in testosterone production and thus a decline in free testosterone levels which may also be accompanied with a rise in estrogen levels also. Around the age of 40 the level of free testosterone begins to decline about 1% a year.
Testosterone levels have been steadily declining even in young men over the years. Yale School of Medicine has presented testosterone levels in young men decreased from 1999-2000 (605.39 ng/dL), 2003-2004 (567.44 ng/dL), 2011-2012 (424.96 ng/dL), 2013-2014 (431.76 ng/dL), and 2015-2016 (451.22 ng/dL). Potential causes for these declines could be increased obesity/BMI, assay variations, diet/phytoestrogens, declined exercise and physical activity, fat percentage, marijuana use, and environmental toxins. A major problem is that official laboratory reference ranges for testosterone in young men have also declined over the years to match this observation so now what is considered normal is in fact low compared to levels 20 years ago thus it is getting more difficult for men to get the treatment they need.
Symptoms of Low Testosterone
Symptoms are: decreased libido, erectile dysfunction, ejaculatory problems, decreased energy and strength, increase in body fat, loss of muscle mass, prostate enlargement, osteoporosis, depression, inability to concentrate, reduced mental agility and loss of enthusiasm.
Men with low testosterone levels also tend to have these heart disease risk factors: angina, atherosclerosis, diabetes, high blood glucose, high cholesterol, high triglycerides, high blood pressure, high level of blood clotting factors, low blood clotting inhibitors and a high body mass index.
Causes of Low Testosterone
The reasons why free testosterone levels decline with age include:
- A protein called SHBG (Sex hormone binding globulin) rises as we age and more testosterone is bound up to it, reducing the amount of free and available testosterone.
- More testosterone may be converted into estrogens by an enzyme called aromatase. Increasing estrogen levels negatively feeds back onto the brain slowing down further testosterone production.
- More testosterone may be converted into dihydrotestosterone (DHT) by an enzyme called 5 alpha reductase.
- Decreased functioning by the aging testicles known as primary hypogonadism.
- Decreased pituitary output of LH hormone which ultimately causes a decrease in stimulation of the testicals to produce testosterone which is known as secondary hypogonadism. Decreased pituitary LH output may be due to decreased hypothalamus stimulation.
- Adrenal fatigue causes a decrease in DHEA production which in turn reduces testosterone production as testosterone is produced from DHEA in the body.
- Xenoestrogens – exposure to estrogen like pollutants in the environment such as certain pesticides (DDT, DDE), petrolum based chemicals (PCB’s, benzene), plastics (PVC), metals (cadmium, arsenic) and hormones from food sources may all cause a negative feedback in the brain which in turn reduces testosterone production in addition to blocking tstosterone receptors.
- Considering the whole being and not only the physical aspect, if a man gives up or withdraws from life due to a number of possible reasons such as he is not content, he may be overwhelmed with life, he lacks true love in his life, etc this withdrawal will then cause low life-force (low kidney energy causing adrenal fatigue) which then causes a vascular contraction. Both low life force and vascular contraction stagnate the testes causing a decrease in testosterone production. Low testosterone is therefore a marker that a man has been living in long term withdrawal or has given up on life. He needs to address his lack of commitment to life! Click here for more information on the emotional cause of hormone imbalances in men.
Diagnosis of Low Testosterone
If you suspect you may have this condition then you should have at least your free testosterone, DHT, SHBG, Estradiol, DHEA and cortisol hormone levels measured. This test will determine if you are testosterone deficient, if a testosterone/estrogen imbalance is present, if estrogens are too high, if SHBG is too high, if DHT is too high and also help diagnose adrenal stress. Thyroid hormone testing is also essential.
Presently there is a real debate as to which method of testing is best. Refer to our article on blood, urine and/or saliva testing for details. Whichever method is used if total testosterone levels are found to be low (<13.9nmol/L) and/or you suffer from symptoms of low testosterone then you need to discuss it with your doctor.
When comparing your baseline test results we do not recommend you use the age adjusted reference ranges as an aging body still requires as much testosterone as a younger body of the same size and height. So called “normal” reference ranges are based on poor science, politics and economics rather than fact and science. “Normal” reference ranges are constantly being adjusted and reduced over time by the so called endocrine experts which is only reflecting the decrease in health and vitality of the average population. When diagnosing a testosterone deficiency your baseline levels should be compared to optimal levels and not “normal” reference range.
To further complicate diagnosis it has been noted by many physicians that men now days require higher levels of testosterone to achieve symptomatic relief due to increasing incidence of testosterone resistance which in part is due to the increased presence of environmental endocrine disruptors and not lower levels which is not being accepted by the medical establishment. A Testosterone Resistance paper published in 2008 concluded that “The many parallels and interactions between maturity onset diabetes and Testosterone deficiency Syndrome (TDS) suggest that a combination of lack of testosterone and its metabolites, combined with resistance to its action at multiple levels, underlies the pathology of androgen deficiency. Just as insulin resistance is thought to vary between tissues, so is androgen resistance, and therefore, different organs may respond functionally.” From their findings they further concluded that “This coincides with the emerging view that “An emphasis and reliance on serum T alone hinders the clinician’s ability to manage testosterone deficiency syndromes (TDS)”. Low total testosterone is just the tip of the iceberg of androgen deficiency.” Their final conclusions were “due to the complexity of factors involved in androgen resistance, and the invalidity of androgen assays, it seems logical to adopt the suggestion endorsed by Black et al., which where typical symptoms or conditions known to be related to androgen deficiency occur, that a 3-month therapeutic trial of testosterone treatment be given.”
Treatment
The approach taken in Testosterone Replacement Therapy (TRT) is to supplement testosterone at the minimum dose required to overcome symptoms. The use of hormone tests to monitor therapy has become controversial as a result of many practitioners dosing patients based on lab test results ignoring the fact that symptoms still remain even though lab results indicate levels are “normal”. They are treating the lab results and not the patient. As mentioned above testosterone resistance and environment androgen blockers are the reason some men need higher levels so lab results cannot be relied upon as the sole means of determining the dose. The minimum dose required to achieve complete elimination of symptoms should be the aim while using test results to ensure levels do not exceed the acceptable range.
It must be noted here that this should not be misinterpreted as we never advocate high, abnormal Testosterone levels.
Maintaining estrogens at the low end of the normal range with aromatase inhibitors has also crept into TRT protocols despite it contradicting the research. The use of aromatase inhibitors is a practice long used by bodybuilders on massive doses of testosterone doses and should not apply to men on TRT. Dr Rouzier has lead the way to debunk this practice in TRT as recent evidence shows E2 levels up to 290pml/L cause no symptoms in men and can be very beneficial for cardiovascular and bone protection. If we inhibit estrogen production then the cardiovascular and bone building benefits of TRT are lost as these benefits are due to the conversion of testosterone into estrogen. We recommend estrogen reduction only if symptoms are present and/or if estradiol exceeds the normal range. These symptoms include: water retention, puffiness, bloating, sensitive nipples, poor erections and moodiness.
Supplementation can be achieved in several ways:
(1) Topical creams/gels are commercially available however these have several issues and not considered ideal.
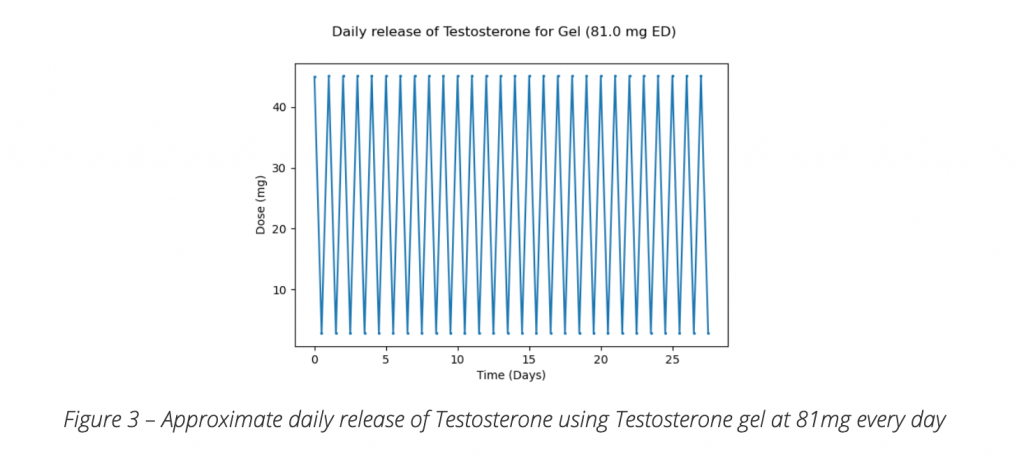
With commercially available Testosterone creams the dose often required to achieve any benefit is 100-200mg a day. Taking into account a healthy man only produces approximately 10mg a day to remain symptom free and maintain healthy levels why is such as large dose required when using creams? The only reasonable explanation is poor absorption and/or rapid elimination. This in itself creates problems as the rapid elimination results in constantly fluctuating levels which some men experience as a see saw effect of their symptoms. The graph below indicates testosterone blood levels while using topical testosterone.
Another issue is to achieve these doses 2 to 4ml of the commercially available cream needs to be applied daily which is a lot of cream to rub in often covering both arms and chest in one application which is very inconvenient. Finally using this amount of cream becomes too expensive for many to be able to afford costing around $60 for a 12 to 25 day supply depending on the dose.
Topical Gels are even less effective. These are alcohol based and once applied the ethanol evaporates within minutes leaving a dry powder residue on the skin which does not absorb as there is no carrier to transport it into the skin so most of the testosterone powder remains on the surface of your skin. If you have used it you will know what I mean.
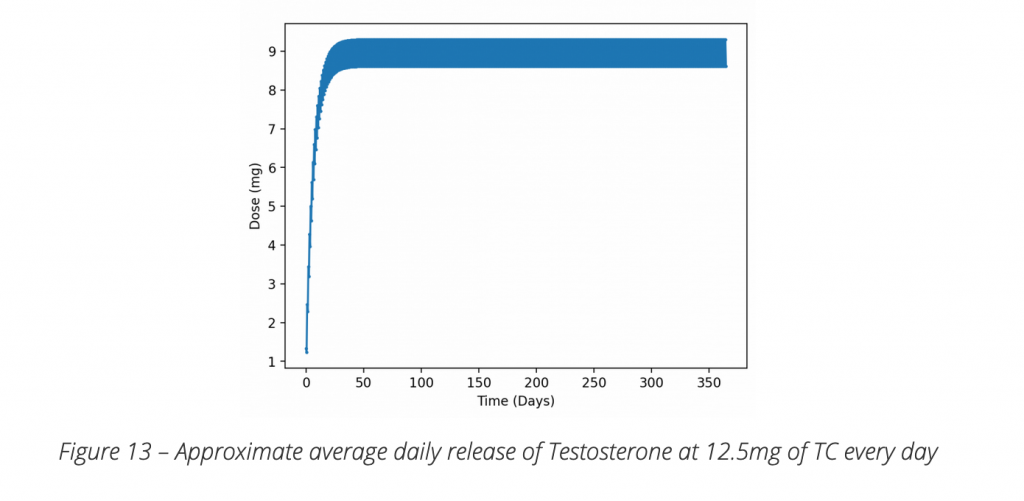
(2) Subcutaneous (SubQ) Injections – Most experienced TRT experts around the globe all agree that SubQ microdosing is the gold standard and the future of TRT as it overcomes all the draw backs of transdermal application. Only small physiological doses comparable to endogenous production are administered either daily or every other day as opposed to large transdermal doses. The release of Testosterone into the blood stream is consistent with no wide fluctuations observed with transdermal application which leads to better control of symptoms. In our experience most men who change over from transdermal creams to SubQ Microdosing cannot believe the improvement and difference in how much better they feel.
Concerns with Testosterone Replacement
In 1941 Higgins published a study where two men were given testosterone (one man had been castrated so not a good test subject) and after 14 days their serum phosphatase levels increased resulting in the conclusion that testosterone causes prostate cancer. This poorly designed study is the reason many doctors to this day believe testosterone causes prostate cancer which was taught to them at University based on this study. There have been NO studies since proving any such link. In actual fact there have been a number of studies showing low testosterone may be responsible for prostate cancer and that testosterone supplementation has no effect on PSA and may actually protect against prostate cancer. Watch the short video below which is one of the leading experts on Testosterone supplementation in the world presenting the research.
Want More Information?
For more information you can access a free online consultation or alternatively speak to your doctor.
Contact Us
In order to obtain more information or alternatively to arrange a consultation you can contact us. You can also click here to find an integrative doctor open to treating this condition.
References
(1) Rhoden, E.L, Risks of Testosterone-Replacement Therapy and Recommendations for Monitoring Ernani Luis Rhoden, M.D., and Abraham Morgentaler, M.D. NEJM Volume 350:482-492 Jan 29, 2004.
(2) Perchersky AV et al. “Androgen administration in middle-aged and aging men: effects of oral testosterone undecanoate on di-hydrotestosterone, oestradiol, and prostate volume.” International J Androl 2002; 25(2): 119
(2A) Marks, Leonard S., Effect of Testosterone Replacement Therapy on Prostate Tissue in Men With Late-Onset Hypogonadism A Randomized Controlled Trial. , MD JAMA. 2006;296:2351-2361.
(2B) Press Release for JAMA , Leonard Marks MD article
(3) https://themenshealthclinic.co.uk/microdosing-trt-the-future-of-testosterone-replacement-therapy/

